13 min read
3 Signs Your Gut-Brain Axis is Overwhelmed
Authored by
Gültekin Daglar
Released on
January 18, 2026
Discover three science-backed signs that your gut-brain axis may be overwhelmed and learn how early intervention through integrative healthcare can restore balance naturally.
You’ve probably experienced it before: that unsettling feeling in your stomach before an important presentation, or the sudden loss of appetite when anxiety strikes. These aren’t coincidences — they’re evidence of one of the most fascinating and clinically significant connections in human physiology: the gut-brain axis.
For decades, we treated the digestive system and the brain as separate entities. Today, a growing body of peer-reviewed research reveals they’re in constant, bidirectional communication. When this communication system becomes overwhelmed, your body sends warning signals that are easy to dismiss — but important to recognise.
Understanding these signs is the first step toward early intervention healthcare, allowing you to address imbalances before they develop into chronic conditions. Here’s what the science tells us about recognising when your gut-brain axis needs support.
Understanding the Gut-Brain Axis: More Than a “Gut Feeling”
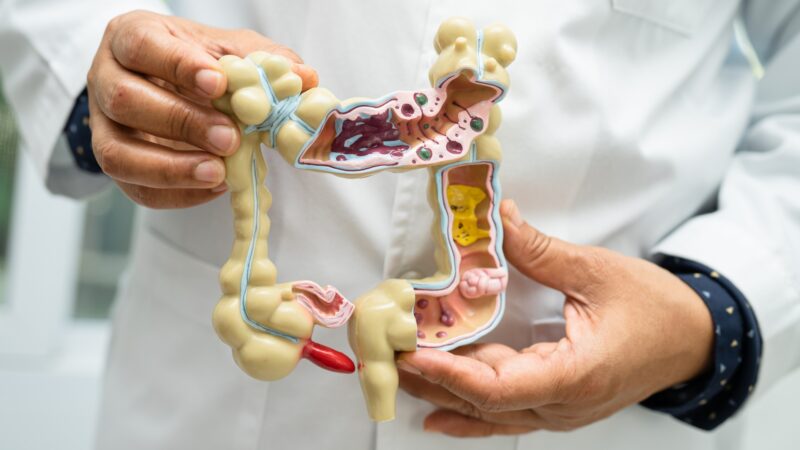
The gut-brain axis refers to the complex communication network linking your gastrointestinal tract to your central nervous system. This connection operates through multiple pathways: the vagus nerve (the longest cranial nerve in the body), the immune system, and the trillions of microorganisms living in your intestines — collectively known as the gut microbiome.
Your gut contains approximately 500 million neurons and produces roughly 95% of your body’s serotonin, often called the “happiness hormone.” This has led researchers to call the gut the “second brain,” or scientifically, the enteric nervous system.
When functioning optimally, this axis supports healthy digestion, stable mood, robust immunity, and clear cognitive function. When overwhelmed — whether by chronic stress, poor diet, medication use, or environmental factors — the consequences ripple through multiple body systems. The key to holistic health lies in recognising these early warning signs and addressing them through an integrative approach that considers the whole person, not just isolated symptoms.
Sign #1: Your Digestive Symptoms Intensify During Stressful Periods
The Connection Between Stress and Digestion
One of the most telling signs of gut-brain axis dysfunction is a clear correlation between your stress levels and digestive symptoms. Perhaps you’ve noticed that during demanding work periods, you experience bloating, constipation, diarrhoea, or abdominal discomfort that seems to resolve when life calms down.
This isn’t psychosomatic — it’s physiological. When your brain perceives stress, it activates the hypothalamic-pituitary-adrenal (HPA) axis, triggering a cascade of hormonal responses. Cortisol and adrenaline flood your system, and blood flow redirects away from digestive organs toward muscles needed for “fight or flight.” Research published in the World Journal of Gastroenterology confirms that chronic stress alters gut motility, increases intestinal permeability (often called “leaky gut”), and disrupts the delicate balance of gut bacteria. Over time, this creates a feedback loop where gut dysfunction further amplifies stress responses.
What to Watch For
- Bloating or cramping that worsens before deadlines or during conflict
- Alternating constipation and diarrhoea linked to emotional states
- Heartburn or acid reflux that flares during anxious periods
- Loss of appetite when stressed, followed by overeating when the pressure subsides
- Nausea without apparent cause during emotionally charged situations
These patterns often precede more serious gastrointestinal conditions. Irritable Bowel Syndrome (IBS), for example, affects an estimated 10-15% of the global population, and research consistently shows a strong stress-gut connection in its development. Recognising the pattern early creates opportunities for intervention before symptoms become entrenched.
Sign #2: Your Mood Fluctuates in Sync with Your Eating Patterns
The Microbiome-Mood Connection
If you’ve noticed that what you eat — or don’t eat — significantly impacts your emotional state, your gut-brain axis may be sending you an important message. This goes beyond the normal energy fluctuation after meals. We’re talking about noticeable mood shifts: increased irritability, unexplained anxiety, or a low mood that lifts after eating certain foods.
The science here is compelling. Your gut microbiome directly influences neurotransmitter production. Certain bacterial strains produce gamma-aminobutyric acid (GABA), a calming neurotransmitter. Others synthesise precursors to dopamine and serotonin. When your microbiome is imbalanced — a condition called dysbiosis — this production can become erratic.
A landmark study in Nature Microbiology analysed data from over 1,000 participants and found consistent links between specific gut bacteria and depression. Participants with depression showed depleted levels of certain beneficial bacteria, regardless of antidepressant use.
What to Watch For
- Feeling anxious or irritable when meals are delayed
- Mood improvements that coincide with eating fermented foods or high-fibre meals
- Sugar cravings that feel compulsive, particularly during low emotional periods
- Brain fog or difficulty concentrating that clears after eating
- Emotional volatility that tracks with dietary changes
The Mind-Body Connection in Practice
This sign highlights why holistic wellness approaches often emphasise nutrition as a foundation for mental health. Rather than treating mood symptoms in isolation, addressing the underlying gut environment can create sustainable improvements that pharmaceutical interventions alone may not achieve. This is where the philosophy of integrative medicine becomes particularly relevant: understanding that mental and physical health are not separate domains, but interconnected systems that influence each other continuously.

Sign #3: You Experience Persistent Fatigue Despite Adequate Rest
When Tiredness Becomes a Warning Sign
Perhaps the most frustrating sign of gut-brain axis overwhelm is chronic fatigue that doesn’t respond to conventional solutions. You’re sleeping seven to eight hours, you’ve reduced caffeine, you’ve even tried sleeping earlier — yet you wake up exhausted, drag through the afternoon, and never quite feel restored.
This type of fatigue often has roots in gut dysfunction. When the intestinal barrier becomes compromised, small amounts of bacterial components can enter the bloodstream, triggering low-grade systemic inflammation. The immune system remains perpetually activated, consuming energy resources and leaving you depleted.
Additionally, an overwhelmed gut-brain axis often means your vagus nerve — the primary communication highway between gut and brain — isn’t functioning optimally. The vagus nerve regulates parasympathetic activity, responsible for “rest and digest” functions. When vagal tone is low, your body struggles to shift out of stress mode, even during sleep. Research in Frontiers in Psychiatry has linked reduced vagal tone to both chronic fatigue and depression, suggesting these conditions may share underlying mechanisms related to gut-brain communication.
What to Watch For
- Waking up tired regardless of sleep duration
- Energy crashes in the early afternoon (beyond normal circadian dips)
- Feeling “wired but tired” — exhausted yet unable to relax
- Post-meal fatigue, especially after eating
- Recovery from illness or exertion taking longer than expected
Chronic fatigue is often dismissed or attributed to “just getting older” or “being too busy.” Yet it frequently represents an early warning sign of systemic imbalance. Addressing it through preventive healthcare approaches — rather than waiting for a diagnosable condition — can prevent years of diminished quality of life.
Why an Integrative Approach Makes a Difference
When the gut-brain axis becomes overwhelmed, no single intervention addresses every contributing factor. This is why many people find that conventional treatments provide partial relief but don’t fully resolve their symptoms. An integrative healthcare approach recognises that restoring gut-brain balance often requires multiple strategies working together: addressing the physical body, supporting the nervous system, and making sustainable lifestyle modifications.
Supporting the Physical Body
Therapies that work directly with the body’s tissues can help restore optimal function. Manual therapies, including massage therapy, improve circulation, support lymphatic drainage, and reduce muscle tension that often accompanies chronic stress. For the gut specifically, certain techniques can help stimulate motility and relieve discomfort.
Naturopathy offers evidence-informed nutritional and botanical support for gut healing. This might include personalised dietary protocols, targeted supplementation to address microbiome imbalances, or herbal medicines that support digestive function and reduce inflammation.
Regulating the Nervous System
Because gut-brain axis dysfunction often involves a dysregulated stress response, therapies that support nervous system balance are particularly valuable. Medical acupuncture, grounded in neurophysiology, stimulates specific points that influence vagal tone and parasympathetic activation. Research published in Evidence-Based Complementary and Alternative Medicine demonstrates acupuncture’s effectiveness for functional gastrointestinal disorders, with mechanisms including modulation of the gut-brain axis. Kinesiology works with the body’s biofeedback systems to identify and address stress patterns held in the body. This approach can uncover contributors to gut-brain imbalance that might not be apparent through conventional assessment.
What these approaches share is a commitment to treating the whole person rather than isolated symptoms. This philosophy — integrating the best of evidence-based conventional medicine with time-tested traditional practices — often yields the most sustainable results for complex conditions like gut-brain axis dysfunction.

Listening to What Your Body is Telling You
Your body communicates constantly. The three signs discussed here — stress-linked digestive symptoms, mood fluctuations tied to eating patterns, and persistent fatigue — represent your gut-brain axis asking for attention.
The good news is that this system is remarkably responsive to the right support. Early intervention, before symptoms become chronic, typically produces faster and more complete recovery than waiting until dysfunction is deeply established. Whether you’re navigating the stress of life transitions, managing the demands of a busy career, or simply wanting to optimise your health for the years ahead, paying attention to these signals is a form of self-care that pays dividends.
Holistic health isn’t about rejecting conventional medicine or embracing unsupported treatments. It’s about recognising the interconnected nature of human physiology and choosing approaches that honour that complexity.
Your gut and brain are having a conversation. The question is whether you’re listening.
Seena Integrative Health Centre offers personalised consultations for those seeking to understand and support their gut-brain health through evidence-based integrative approaches. Our team combines scientific rigour with a commitment to whole-person care, helping you move from symptom management to lasting wellness.



